Understanding OCD Panic Attacks: Symptoms, Causes, and Effective Treatment Strategies
Obsessive-compulsive disorder (OCD) can sometimes produce intense panic attacks when intrusive thoughts or blocked compulsions trigger a rapid physiological fear response. This article explains what OCD panic attacks are, why intrusive thoughts escalate to full panic, how to distinguish those events from panic disorder or generalized anxiety, and which evidence-based treatments and daily coping tools reduce both obsessional distress and panic reactivity.
Readers will gain practical steps for calming an acute OCD-triggered panic attack, clear diagnostic cues that clinicians use to differentiate conditions, and a comparison of treatments from CBT and ERP to medications and intensive residential care. We’ll also cover safe coping techniques that avoid reinforcing compulsions, strategies for relapse prevention, and signs that indicate higher levels of care may be necessary. Finally, the guide describes how integrated residential programs approach complex OCD-panic presentations and where to find specialized support. Understanding these links between intrusive thoughts, compulsive urges, and panic physiology is the first step toward choosing interventions that break the OCD–panic cycle and restore daily functioning.
What Are OCD Panic Attacks and How Do They Manifest?
OCD panic attacks occur when an obsessional fear or intrusive thought triggers sudden, intense physiological arousal accompanied by an urge to perform a compulsion for relief. The mechanism begins with an intrusive thought that is catastrophically appraised, producing escalating anxiety and activating the sympathetic nervous system; if a compulsion is blocked or fails to reduce uncertainty, the anxiety can peak into a panic attack.
Clinically, this manifests as both the cognitive distress of obsessional themes and the classic panic symptoms—rapid heart rate, shortness of breath, dizziness—creating a compound episode that feels qualitatively different from either pure OCD or isolated panic disorder. Recognizing this mixed presentation helps guide treatment toward approaches that simultaneously target intrusive cognitions and panic physiology, and it sets the stage for comparing OCD panic with other anxiety conditions below.
What Is Obsessive-Compulsive Disorder and Its Role in Panic Attacks?
Obsessive-compulsive disorder is characterized by recurring intrusive thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to reduce distress or prevent feared outcomes. Obsessions are typically experienced as unwanted and highly distressing, prompting compulsions that temporarily lower anxiety but reinforce the obsession-compulsion link over time. When compulsions are prevented—by circumstance, choice, or treatment—the resulting intolerance of uncertainty and amplified anxiety can precipitate panic-level arousal. Understanding OCD’s core dynamics explains why treatment must both reduce intrusive thought frequency and increase tolerance of distress to prevent panic escalation.
How Do Intrusive Thoughts Trigger Panic Attacks in OCD?
Intrusive thoughts become panic triggers when they are appraised as immediate threats, leading to catastrophic thinking and physiological arousal that outstrips usual coping resources. Common intrusive themes—harm, contamination, sexual or moral fears—can provoke urgent mental rituals or checking; when the person cannot perform the ritual, anxiety spikes and the body responds with panic symptoms. A typical progression is: intrusive thought → catastrophic interpretation (“I might cause harm”) → rising anxiety → urge to neutralize → inability or refusal to neutralize → panic. Recognizing this cascade helps target both the appraisal (through cognitive techniques) and the physiological response (through grounding and breathing).
What Are the Common Symptoms of OCD Panic Attacks?
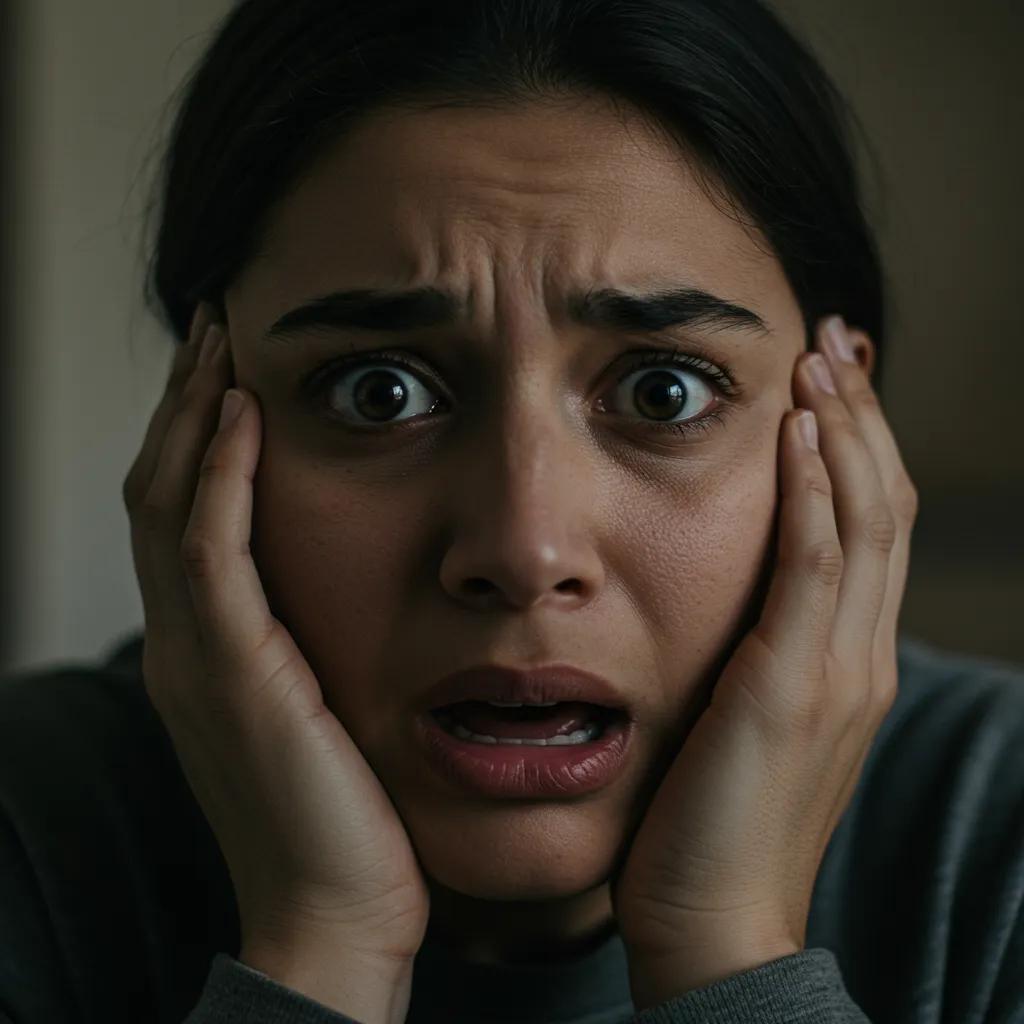
OCD-related panic attacks combine cognitive features of OCD with the somatic signs of panic, producing a distinct symptom cluster that clinicians can use to identify mixed episodes. Physical symptoms commonly include tachycardia, shortness of breath, trembling, sweating, dizziness, and a sense of impending doom; cognitive symptoms include intrusive imagery, fixation on feared outcomes, intense guilt or shame, and overwhelming urges to perform compulsions. Behaviorally, individuals may attempt covert mental rituals, seek reassurance, or avoid triggering situations—each of which can briefly reduce anxiety but perpetuate long-term vulnerability to panic. Awareness of both domains—thought content and bodily arousal—guides immediate coping and longer-term therapy.
How Does the OCD-Panic Attack Cycle Work?
The OCD–panic cycle is a feedback loop in which obsessional thoughts provoke anxiety, compulsions temporarily relieve distress, and relapse or prevention of compulsion leads to escalating panic that reinforces avoidance. Step 1: an intrusive thought captures attention; Step 2: catastrophic appraisal amplifies fear; Step 3: a compulsion is executed or sought to reduce distress; Step 4: relief occurs but is short-lived, increasing the likelihood of future panic when compulsions are not available. Breaking the cycle requires interventions that reduce the power of intrusive thoughts (cognitive restructuring), reduce reliance on compulsions (exposure and response prevention), and teach distress tolerance for physiological panic responses. Interrupting a single link—especially the compulsion—changes the long-term reinforcement pattern and lowers panic risk.
How Can You Differentiate OCD Panic Attacks from Panic Disorder and Anxiety Attacks?
Differentiating OCD panic attacks from panic disorder or general anxiety involves examining trigger specificity, presence of compulsive responses, and temporal patterns of worry and fear. OCD-triggered panic is typically tied to intrusive content and an urge to neutralize, whereas panic disorder involves spontaneous or situational panic often without obsessional themes, and generalized anxiety disorder produces persistent, diffuse worry rather than discrete panic episodes. Assessing whether the panic follows an intrusive thought, whether rituals or reassurance-seeking follow the episode, and whether worry is pervasive or event-linked helps clinicians choose ERP and CBT strategies over panic-focused treatments alone. The following table summarizes diagnostic clues for quick clinical comparison.
Different conditions present with distinguishable clinical features useful for diagnosis and treatment planning.
| Condition | Core feature | Diagnostic clue / typical symptom |
|---|---|---|
| Obsessive-Compulsive Disorder (OCD) | Intrusive obsessions + compulsions | Panic follows specific intrusive thoughts and is accompanied by urges to perform rituals |
| Panic Disorder | Recurrent unexpected panic attacks | Panic often occurs without clear obsessional trigger and leads to fear of future attacks |
| Generalized Anxiety Disorder (GAD) | Chronic, diffuse worry | Persistent worry across domains without discrete obsession-compulsion episodes |
What Are the Key Differences Between OCD, Panic Disorder, and Generalized Anxiety Disorder?
OCD centers on intrusive thoughts and compulsive behaviors; panic disorder centers on recurrent panic attacks and fear of recurrence; GAD centers on persistent, excessive worry across multiple areas. Clinicians look for whether behaviors aim to neutralize obsessions (OCD), whether panic appears unexpectedly or in specific contexts (panic disorder), and whether anxiety is generalized and chronic (GAD). Treatment implications follow: ERP and OCD-focused CBT are primary for OCD with panic, while interoceptive exposure and panic-focused CBT target panic disorder, and cognitive strategies and worry-management address GAD. Accurate diagnosis often requires careful history-taking about triggers, rituals, and avoidance patterns.
How Do OCD Panic Attacks Differ from Anxiety Attacks?
OCD panic attacks differ from generic anxiety attacks in trigger specificity and behavioral responses: anxiety attacks often arise from situational stress or build-up of worry, while OCD panic is directly tied to intrusive thoughts and results in compulsive urges. In OCD panic, the cognitive focus is narrow and obsession-driven, which makes avoidance and ritualization especially likely; in general anxiety attacks, symptoms may be diffuse and tied to life stressors or chronic worry. Physically both can share tachycardia and breathlessness, but the presence of ritualistic attempts to reduce the thought-driven distress strongly indicates OCD-related panic instead of an anxiety attack.
Can OCD and Panic Disorder Co-occur? What Does Comorbidity Mean?
Yes, OCD and panic disorder can co-occur; comorbidity means two diagnostic conditions exist simultaneously and often complicate the clinical picture and treatment. When comorbidity is present, panic attacks may be both spontaneous and triggered by obsessions, requiring integrated treatment that addresses interoceptive sensitivity alongside compulsive behaviors. Prevalence studies show notable overlap among anxiety-spectrum disorders, and comorbidity typically predicts greater severity and functional impairment. Treatment planning for comorbid cases emphasizes coordination between medication management, CBT/ERP for OCD, and panic-specific exposure techniques to address both spontaneous and obsession-triggered panic.
What Are the Most Effective Evidence-Based Treatments for OCD Panic Attacks?
Effective treatment for OCD panic attacks combines interventions that reduce intrusive thoughts, prevent compulsive responses, and directly address panic physiology; core options include CBT with ERP, DBT skills training, selective serotonin reuptake inhibitors (SSRIs), and, for severe cases, structured residential programs. ERP is the gold-standard behavioral treatment for OCD and reduces the need for compulsions that fuel panic, while CBT addresses catastrophic appraisals that convert intrusive thoughts into panic triggers. DBT contributes emotion regulation and distress tolerance skills to manage acute panic without reverting to rituals, and SSRIs can reduce baseline obsessional intensity and panic frequency under psychiatric supervision. The table below compares these approaches by mechanism and practical benefit.
Below is a concise comparison of major treatments, how they work, and what they achieve for OCD-related panic.
| Treatment | Mechanism | How it helps OCD panic attacks |
|---|---|---|
| Exposure and Response Prevention (ERP) | Graded exposure to obsessions + prevention of compulsions | Reduces compulsion-driven panic by increasing tolerance of distress and uncertainty |
| Cognitive Behavioral Therapy (CBT) | Cognitive restructuring + behavioral experiments | Lowers catastrophic appraisal and teaches coping skills to reduce panic escalation |
| Dialectical Behavioral Therapy (DBT) | Distress tolerance + emotion regulation skills | Provides strategies to tolerate acute panic without performing compulsions |
| SSRIs (medication) | Neurochemical modulation of serotonin pathways | Decreases baseline obsessional intensity and panic vulnerability as adjunct to therapy |
| Residential/Inpatient Treatment | Intensive, multidisciplinary care with 24/7 support | Offers structured environment for intensive ERP, medication adjustments, and stabilization |
How Does Cognitive Behavioral Therapy Help Manage OCD Panic Attacks?
Cognitive behavioral therapy reduces panic by challenging catastrophic interpretations of intrusive thoughts and teaching behavioral experiments that disconfirm feared outcomes. CBT techniques—cognitive restructuring, thought records, and behavioral activation—help patients reframe intrusive content and reduce rumination that fuels physiological arousal. In practice, therapists guide clients in identifying automatic catastrophic appraisals during panic, testing alternative predictions, and practicing opposite behaviors to weaken fear associations. Over weeks to months, CBT diminishes panic reactivity by altering both thought patterns and avoidance behaviors, and it directly complements ERP work aimed at breaking ritual cycles.
What Is Exposure and Response Prevention and Why Is It the Gold Standard?
Exposure and Response Prevention involves deliberately and gradually confronting obsessional triggers while refraining from the compulsive response, allowing habituation to anxiety and correction of threat overestimation. ERP’s graded exposures lower the fear response by demonstrating that feared consequences are unlikely or tolerable and that distress naturally declines without rituals. For OCD-triggered panic, ERP is particularly powerful because it prevents compulsions that temporarily relieve anxiety and thereby remove the reinforcement loop that escalates panic. Clinician-guided pacing, safety planning, and tolerable intensity levels ensure exposures are effective without overwhelming the patient.
How Does Dialectical Behavioral Therapy Support OCD and Panic Symptoms?
Dialectical Behavioral Therapy contributes emotion regulation, mindfulness, and distress tolerance skills that help people withstand panic without reverting to compulsions. DBT modules teach techniques such as urge-surfing, paced breathing, and radical acceptance—skills that allow a person to observe panic sensations nonreactively and avoid performing rituals. When integrated with CBT and ERP, DBT provides the moment-to-moment skills needed during exposures and supports relapse prevention by strengthening coping under stress. Clinicians often add DBT when emotion dysregulation, self-harm risk, or severe distress tolerance deficits complicate OCD treatment.
What Role Do Medications Like SSRIs Play in Treating OCD Panic Attacks?
SSRIs are often used as first-line pharmacotherapy to reduce obsessional intensity and lower baseline anxiety, making behavioral treatments like ERP more tolerable and effective. By modulating serotonin pathways, SSRIs can decrease intrusive thought frequency and blunt panic reactivity, but medication is most effective when combined with structured psychotherapy. Psychiatric oversight is essential: clinicians tailor dosing, monitor response, and consider adjunctive options when treatment resistance or severe panic persists. Medication alone rarely resolves the cycle of compulsions and panic; it is a tool that enhances engagement in ERP and cognitive work.
What Practical Coping Strategies Can Help Manage OCD Panic Attacks Daily?

Daily coping strategies should reduce acute panic without reinforcing compulsions and should be practiced in ways that complement long-term therapy goals. Techniques that target breathing, grounding, cognitive defusion, and distress tolerance help de-escalate panic while intentionally avoiding rituals that provide temporary relief. Regular practice of these skills lowers baseline arousal, improves interoceptive tolerance, and prepares someone to engage more effectively in ERP sessions. The table below summarizes practical techniques, their type, and guidance on safe use so users can choose tools that reduce panic while preserving therapeutic progress.
This table helps select coping tools that reduce panic safely without strengthening compulsive patterns.
| Technique | Type | When/how to use it safely |
|---|---|---|
| 4-4-8 breathing | Breathing exercise | Use during early panic onset to reduce physiological arousal; avoid as avoidance of exposure |
| 5-4-3-2-1 grounding | Sensory grounding | Use in public or private to reorient attention to the present and interrupt escalation |
| Urge surfing | Distress tolerance | Apply to observe and ride out compulsion urges without acting; combine with delay tactics |
| Cognitive defusion (labeling thoughts) | Cognitive technique | Use to reduce belief in intrusive thoughts by naming them as “just thoughts” |
| Progressive muscle relaxation | Relaxation | Practice regularly to lower baseline tension; not during ERP exposure sessions |
How Can Mindfulness and Relaxation Techniques Reduce Panic Symptoms?
Mindfulness and brief relaxation practices reduce panic by shifting attention away from catastrophic appraisals and lowering sympathetic arousal through focused breath and body awareness. Short practices—three-minute breathing exercises, a brief body scan, or anchored mindfulness of breath—interrupt rumination and provide physiological down-regulation that reduces the intensity of panic sensations. Regular practice strengthens the ability to observe intrusive thoughts without reacting, which supports ERP goals by increasing tolerance for distress. Practitioners should avoid using mindfulness as avoidance of exposures; instead, integrate it as a complementary skill that prepares the nervous system for therapeutic work.
- Mindfulness offers immediate orientation and long-term resilience when practiced consistently.
- Use short exercises in moments of early distress to prevent escalation.
- Combine mindfulness with behavioral exposure rather than using it to sidestep feared situations.
These practices lower arousal and improve tolerance for anxiety, which makes therapeutic exposures and daily functioning more manageable.
What Are Specific Grounding Techniques to Calm an OCD Panic Attack?
Grounding techniques re-establish a sense of safety by anchoring attention in the present through sensory input, breathing, and muscle engagement. The 5-4-3-2-1 sensory method, paced diaphragmatic breathing, and progressive muscle relaxation are quick, adaptable strategies that work in both public and private settings to interrupt panic’s upward spiral. For public settings, sensory grounding (e.g., feeling a pocket object, naming visible colors) is discreet and effective; at home, full body scans or muscle relaxation can provide deeper physiological relief. Importantly, grounding should be used to reduce panic without becoming a ritualized compulsive avoidance—practitioners should monitor whether grounding is being used to bypass exposures and adjust accordingly.
How to Avoid Compulsions While Managing Panic During OCD Episodes?
Avoiding compulsions during panic requires concrete tactics that increase the delay between urge and action and substitute safe, non-reinforcing responses. Strategies include urge-surfing to watch urges rise and fall, the “delay and distract” method to postpone rituals for defined intervals, cognitive defusion to label intrusive thoughts as transient, and setting behavioral limits agreed with a therapist. Practicing these tactics in low-stakes situations builds confidence for higher-intensity moments and reduces the reinforcement loop that turns compulsions into panic triggers. If urges remain overwhelming despite these tactics, it indicates a need for clinician-supported ERP intensification or higher-level care.
When Should You Seek Professional Help for OCD Panic Attacks?
Professional help is warranted when panic attacks are frequent, disabling, accompanied by suicidal thoughts, resistant to outpatient care, or when compulsions significantly disrupt daily functioning. Key red flags include escalating panic despite self-help, inability to leave the home, severe avoidance, medication side effects, and co-occurring mood symptoms that increase risk. Levels of care range from outpatient CBT/ERP to intensive outpatient programs (IOP), residential inpatient treatment, and hospital-based care for acute safety concerns. Recognizing when outpatient strategies are insufficient helps patients access timely, appropriate care that prevents deterioration and supports sustained recovery.
- Seek higher-level care when safety is a concern or symptoms prevent basic functioning.
- Consider intensive programs when panic and compulsions are treatment-resistant or severely impairing.
- Engage family or close supports when accommodation and avoidance patterns maintain symptoms.
Early triage into the correct level of care shortens the time to stabilization and creates a platform for durable recovery.
What Are the Benefits of Residential Inpatient Treatment for Severe OCD and Panic Attacks?
Residential inpatient treatment provides a structured environment for intensive therapy, uninterrupted practice of ERP, medication management, and 24/7 clinical support that stabilizes severe or treatment-resistant presentations. In a residential setting, patients receive concentrated daily therapy hours, immediate clinician access during crises, and supervised opportunities to practice exposures without daily life constraints that might otherwise enable avoidance. This environment is especially useful for individuals with severe comorbidity, high avoidance, or repeated failed outpatient attempts, because it allows clinicians to titrate interventions and observe progress in real time. The enclosed setting accelerates skill acquisition and supports medication adjustments while minimizing external triggers that can undermine treatment.
How Does 24/7 Support and Personalized Care Improve Recovery Outcomes?
Continuous clinical availability and personalized treatment planning improve outcomes by ensuring consistent application of therapeutic principles, swift crisis management, and coordinated medication oversight. Personalized plans are built from diagnostic assessment, symptom severity, and individual triggers; ongoing monitoring allows clinicians to adapt exposures, pacing, and adjunctive skills training for maximal benefit. 24/7 support shortens crisis windows, prevents maladaptive coping from becoming ingrained, and enables therapists to model and reinforce new behaviors—accelerating stabilization and skill generalization back into daily life. This intensity often produces quicker reductions in panic frequency and compulsive responding compared with fragmented outpatient scheduling.
How Is Family Involvement Important in Long-Term OCD Panic Attack Recovery?
Family involvement reduces accommodation, supports relapse prevention, and improves generalization of therapeutic gains by educating loved ones about how to respond to obsessions and panic without enabling rituals. Family therapy and psychoeducation teach relatives to set boundaries, avoid reassurance provision, and use supportive coaching during exposures—actions that directly reduce reinforcement of compulsions. Practical family strategies include planned exposure participation, communication scripting during crises, and collaborative relapse-prevention planning. When families understand the OCD–panic cycle and their role in recovery, outcomes improve through a more supportive, consistent environment for applied practice.
After describing levels of care and family roles, it is appropriate to note residential options for severe cases and how integrated programs implement those practices.
For individuals whose OCD and panic symptoms are severe, persistent, or resistant to outpatient care, residential inpatient treatment offers an intensive, structured path to stabilization and skill acquisition. Revival Mental Health provides residential inpatient care that combines evidence-based therapies (CBT, ERP, DBT) with medication management, 24/7 clinical oversight, and holistic supports such as mindfulness and art therapy, all delivered by a multidisciplinary team of on-site psychiatrists and master’s- or doctorate-level clinicians. These program features are designed to create a safe, consistent environment for intensive ERP and for families to engage in treatment planning and relapse prevention.
How Does Revival Mental Health Approach Treatment for OCD Panic Attacks?
Revival Mental Health uses an integrated residential model that pairs evidence-based therapies with holistic supports and continuous clinical oversight to address complex OCD and panic presentations. Their described approach emphasizes intensive, personalized plans overseen by on-site psychiatrists and advanced clinicians, with daily therapy, medication management, and therapeutic activities designed to reduce both obsessional intensity and panic reactivity. Holistic components like mindfulness and art therapy are integrated with CBT, ERP, DBT, and Acceptance and Commitment Therapy to build distress tolerance and long-term relapse prevention skills. This multidisciplinary structure supports stabilization, skill generalization, and family involvement in recovery planning.
What Evidence-Based and Holistic Therapies Does Revival Integrate?
According to program descriptions, Revival integrates CBT, ERP, DBT, and ACT as core evidence-based components, alongside holistic modalities such as mindfulness and art therapy to support emotional processing. This blend targets intrusive thoughts and compulsive behavior (via ERP and CBT), strengthens distress tolerance and emotion regulation (via DBT and ACT), and uses mindfulness-based practices to improve present-moment awareness and reduce reactivity. Art therapy and other holistic supports provide nonverbal avenues for processing trauma or shame that often accompany OCD, complementing the more structured exposures and cognitive work. Multidisciplinary oversight ensures these modalities are coordinated in a cohesive treatment plan.
How Does Revival’s Residential Program Address Complex OCD and Panic Symptoms?
The residential program’s features—intensive therapeutic hours, continuous clinician availability, structured daily routines, and on-site psychiatry—create conditions for concentrated ERP practice and medication optimization. Personalized treatment plans are built from individual assessments and adjusted in real time by a team that monitors response and safety, allowing for graduated exposures in a controlled environment. Continuous support reduces the risk of avoidance and accommodation, and supervised practice accelerates acquisition of coping skills that translate to community settings. Family involvement and relapse-prevention planning are emphasized to support long-term recovery after discharge.
What Success Stories Illustrate Effective OCD Panic Attack Management at Revival?
Specific patient testimonials are not provided here; however, program-level descriptions emphasize stabilization through intensive, coordinated care and multidisciplinary oversight that enable individuals with complex OCD and panic symptoms to make measurable progress. Anonymized program summaries typically highlight reductions in compulsive frequency, improved distress tolerance, and successful transitions to outpatient follow-up after completing residential treatment. Prospective patients and families are encouraged to inquire directly with the program for detailed information about outcomes, individualized pathways, and family engagement options.
What Are Common Questions About OCD Panic Attacks?
This section addresses frequently asked, high-value questions in concise, actionable answers to guide immediate coping and next steps for people experiencing OCD-triggered panic. Each response highlights practical steps, diagnostic clarity, and threshold cues for professional care to fit real-world decision-making.
How Do You Calm an OCD Panic Attack Quickly?
Calm an OCD panic attack by stabilizing physiology, grounding attention, and resisting compulsive responses; immediate steps include slow diaphragmatic breathing, a brief grounding sequence, and cognitive labeling of the intrusive thought. First, take 4–6 slow diaphragmatic breaths to reduce heart rate and breathlessness. Second, use a 5-4-3-2-1 grounding exercise—name five things you see, four you can touch, three you hear, two you smell, one you taste—to reorient sensory focus. Third, label the experience (“I am having a panic response to an intrusive thought”) and use urge-surfing to tolerate the compulsion urge without acting. These steps reduce acute physical symptoms while preventing reinforcement of compulsive behavior; seek professional help if panic recurs or intensifies.
Can OCD Cause Panic Attacks?
Yes—OCD can cause panic attacks when intrusive thoughts are catastrophically misinterpreted and compulsions are blocked or ineffective, producing intense physiological arousal. Intrusive content that is appraised as immediate threat activates the sympathetic nervous system; if the individual cannot neutralize the threat via compulsions, anxiety escalates into panic. This pathway explains the frequent comorbidity and the need to address both cognitive appraisals and behavioral responses in treatment. Integrated intervention reduces both the frequency of intrusive thoughts and the likelihood that those thoughts trigger panic.
What Is the Difference Between an OCD Attack and a Panic Attack?
An “OCD attack” centers on obsessional content and an urge to perform rituals, whereas a “panic attack” centers on sudden intense fear with dominating physical symptoms; the two can overlap when obsessions provoke panic-level arousal. OCD attacks typically involve repetitive mental or behavioral attempts to mitigate a feared outcome, while panic attacks focus on bodily sensations and catastrophic fear about immediate danger. When both occur together, treatment must target the obsession-compulsion cycle and the body’s panic response simultaneously.
How Do Intrusive Thoughts Lead to Panic Attacks in OCD?
Intrusive thoughts lead to panic through a cognitive–physiological cascade: the thought is appraised as threatening, which raises anxiety and sympathetic arousal, and if the urge to neutralize cannot be satisfied a panic attack may follow. Catastrophic appraisal magnifies threat perception, attention narrows to feared outcomes, and physiological symptoms escalate—forming a feedback loop that compounds fear. Interventions that reframe appraisals, increase tolerance of uncertainty, and reduce compulsive responses interrupt this pathway and lower panic risk.
Learn more about specialized residential OCD and anxiety treatment options, including intensive residential inpatient programs that combine evidence-based therapies, medication management, and 24/7 clinical support, by contacting Revival Mental Health for program details and next-step guidance.




